
Tips to stay alcohol free
It can feel difficult to avoid alcohol, but we have tips to help you stay alcohol-free during pregnancy.
There's no safe time or amount of alcohol to drink during pregnancy. Even small amounts of alcohol can harm the development of an unborn baby and have lifelong impacts. It is recommended that women who are pregnant or planning a pregnancy should not drink alcohol to reduce risk of harm to their unborn child.

Alcohol is a teratogen, which means it can interrupt the normal development of an unborn baby.1
Alcohol use at any time during pregnancy can cause:2,3
The risk of harm to a baby increases the more alcohol a mother drinks, and the more frequently she drinks.
It’s never too late to stop drinking – every effort made to stop or reduce lowers the risk of harm to the baby and benefits the mother’s health.
Help is available - for confidential, non-judgemental telephone counselling, information and referrals in Western Australia, click here.
Fetal Alcohol Spectrum Disorder (FASD) is a range of permanent and lifelong conditions that can result from a baby being exposed to alcohol in-utero.
The potential outcomes for a baby exposed to alcohol during pregnancy can fall along a continuum, ranging from mild to more severe.4 People with FASD will have strengths and difficulties in different areas, and this depends on the parts of the brain that have been most damaged by exposure to alcohol.5
Some problems people with FASD might experience can include:
FASD may not be seen at birth and can often go unnoticed until childhood and adolescence when social and behavioural problems become more evident.7
People with FASD can have problems at school, difficulties gaining employment, social exclusion, mental health issues, alcohol and other drug use, and early and repeated engagement with the justice system.11,12
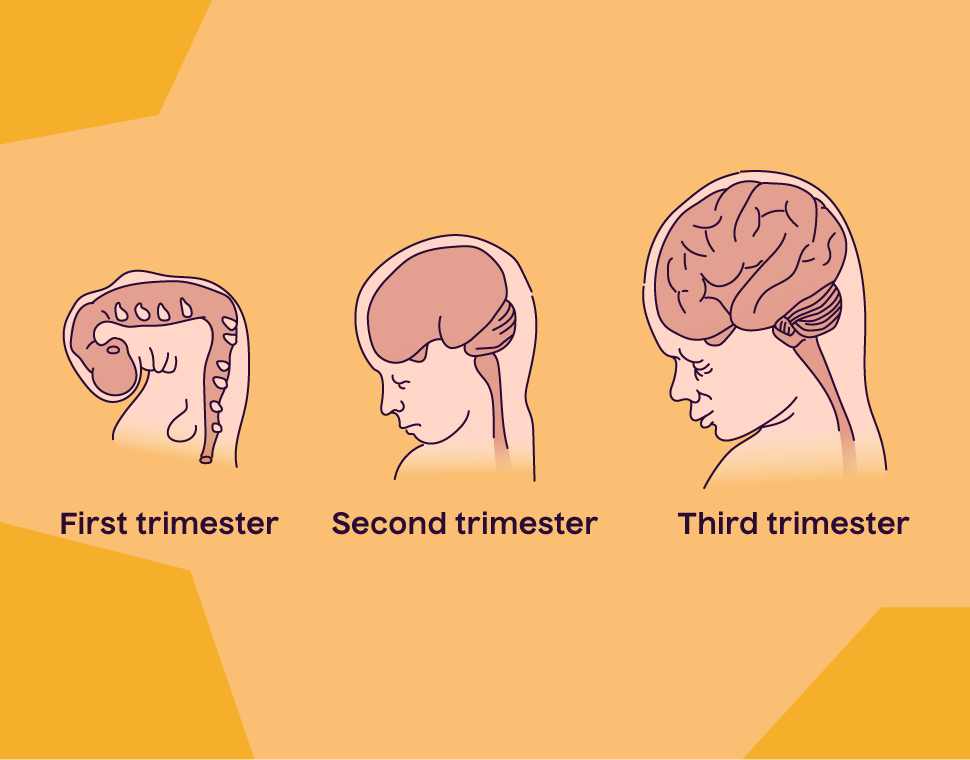
A baby’s brain begins developing early and continues throughout pregnancy. Drinking alcohol during pregnancy can affect brain development during all three trimesters.2
The placenta links the mother’s blood supply to the blood supply of the unborn baby. This means any alcohol mum drinks, the baby drinks too.2
Because the liver of an unborn baby is not fully formed, the baby cannot process alcohol.12 The blood alcohol levels of the mother and the baby are similar.
No. There is no known safe amount of alcohol to drink during pregnancy. Alcohol use, even at low levels, can impact the development of an unborn baby, resulting in lifelong consequences.12 The risk of harm to the unborn baby increases with the more alcohol, and the more frequently, the mother drinks.
Every effort to stop or reduce alcohol use lowers the risk of harm to the baby.
Do you need help for your alcohol use? The Alcohol and Drug Support Line is a confidential, non-judgemental telephone counselling, information and referral service for anyone in WA - find more info here.
Drinking alcohol at any time during pregnancy can harm a developing baby. This is because alcohol is a teratogen - an agent that can interrupt the development of an embryo or fetus.
A baby’s brain grows and develops throughout pregnancy, and alcohol can interfere with the chemicals necessary for normal brain development.
The developing brain of a baby is more vulnerable to damage than the mature brain of an adult.
It’s never too late to stop drinking – every effort made to stop or reduce lowers the risk of harm to the baby and benefits the mother’s health.
Many women are unaware they are pregnant up until the fourth to sixth week of pregnancy, during which time the developing baby is very sensitive to the effects of alcohol. The best advice is to avoid any alcohol use when you start trying to get pregnant.
To reduce the risk of harm to their unborn child, women who are pregnant should not drink alcohol.
Any alcohol the mother drinks passes straight through the placenta to the developing baby, and while the mother might not feel the effects of a few sips or one drink, the baby does.
It may feel difficult to not drink alcohol during pregnancy, particularly if people aren’t aware of your pregnancy yet, but choosing not to drink removes the risk of any potential harm to the baby.
No. The placenta links the blood supply of the mother to the blood supply of the unborn baby and is essential for the growth of a healthy baby. This means if a woman drinks alcohol during pregnancy, the blood alcohol levels of the mother and the baby are similar.
If a woman was drinking alcohol before finding out about pregnancy, it does not automatically mean the baby will be harmed.
If you or someone you know is pregnant, or concerned that alcohol has been consumed in early pregnancy, try to stay alcohol-free, make an appointment to speak with your health care professional.
Every pregnancy is different and there are a range of factors that play a role in determining the risk of harm to the baby.
Yes. If you are pregnant and finding it difficult to manage your drinking, you’re not alone.
It is recommended women contact their health care professional (doctor, midwife, obstetrician or community health nurse) for support and appropriate referral to services.
The Alcohol and Drug Support Line is a confidential, non-judgemental telephone counselling, information and referral service for anyone in Western Australia seeking help for their own or another person’s alcohol or drug use. Find more info here.
The National Health and Medical Research Council recommend for breastfeeding women, not drinking is safest for the baby.
More information on alcohol use and breastfeeding.
While they are legally classified as non-alcohol, some zero-alcohol products still contain a small amount of alcohol.
Alcohol is a teratogen, which means it can interfere with the development of an unborn baby. Therefore there is no safe amount of alcohol use during pregnancy, and zero-alcohol products should be avoided if possible.
Bower, C., Watkins, R., Mutch, R., Marriott, R., Freeman, J., Kippin, N., … & Giglia, R. Fetal alcohol spectrum disorder and youth justice: a prevalence study among young people sentenced to detention in Western Australia. 2018. BMJ Open, 8
Symons, M., Pedruzzi, R., Bruce, K., & Milne, E. A systematic review of prevention interventions to reduce prenatal alcohol exposure and fetal alcohol spectrum disorder in indigenous communities. 2018. BMC Public Health, 18(1227).
Burd, L., Blair, J., & Dropps, K. Prenatal alcohol exposure, blood alcohol concentrations and alcohol elimination rates for the mother, fetus and newborn. 2012. Journal of Perinatology, 32, 652-659.
Page last updated24 October 2023